
My name is Jerad Green, and I was diagnosed with congestive heart failure.
Before my diagnosis, I lived a busy, stressful life, which ultimately impacted not only how I managed my heart failure, but my values as a patient advocate today.
My Symptoms and Journey to a Proper Regimen
I first started developing symptoms that I thought were allergies. I had a stuffy nose, my throat hurt, and I felt a lot of congestion. After taking allergy medication for several weeks, I didn't improve. My symptoms had worsened to experiencing shortness of breath and a loss of appetite. I consulted with a few different doctors using Doctor on Demand. They prescribed me steroids and antibiotics, but my condition continued to worsen.
After seeing different doctors, visiting the emergency room, being misdiagnosed and prescribed medications that were not helpful, I went back to the emergency room and was diagnosed with congestive heart failure and prescribed the typical regimen of medications for heart failure patients. The day after I picked up my prescriptions and started taking them, I ended up returning to the emergency room because my blood pressure had bottomed out with a reading of 60/30. It turns out I had a sensitivity to the drastic change in medications. With the help of my heart failure doctor at the time, I was able to scale back the medications I was given and remained stable, or so I thought.

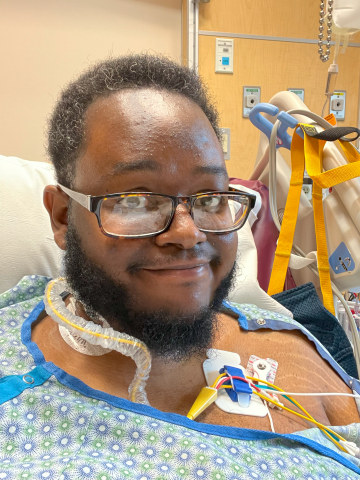
When I moved from South Carolina back to Minnesota and found a new heart failure doctor, tests showed even though I was taking these medications, my B-type Natriuretic Peptide (BNP) had worsened compared to when I was initially diagnosed. Later that week, I was scheduled to get a right heart catheterization to find a therapeutic level of medication that would help my heart function. The new medication regimen I was prescribed helped me feel better, and I improved enough to start cardiac rehab a couple of months later. During this time, my doctors wanted to see if medications and lifestyle changes would improve my ejection fraction to a level where an implantable cardioverter defibrillator (ICD) wasn't necessary. However, I eventually had an ICD placed and that was a bittersweet experience. I had a lot more confidence in my health. I wasn't as worried about my heart because I saw my ICD as a safety net, but my recovery from this surgery took several weeks. At that time, I couldn't attend cardiac rehab, which made it difficult to remotivate myself and continue with healthy habits.
My Life After Being Properly Treated
Looking at my life now, I have a lot more energy. I can push a little more without feeling badly. Movement is easier now than before the medications and procedure, and I feel like I am in general, taking better care of myself. I'm able to set better boundaries, in all spaces of my life to maintain a good sense of health. There are a lot of physical benefits, but also a lot of emotional and mental health benefits that are just as important.
My Advice for Heart Failure Patients
Ignorance is not always bliss. My heart failure diagnosis was completely unexpected and challenging for me to process, but I'm glad that I found out so I could get treated. Don't downplay or minimize the symptoms you are experiencing. I would encourage folks to get checked out because it can save your life. Too many people die in this country from heart disease, especially those in the Black population. They're being left undiagnosed and underdiagnosed for conditions like heart failure.
I also recommend that people invest in alternative spaces of support and healing. My medications have helped me to stabilize and improve my heart function, and there might be alternative ways to supplement our healing as well. Homeopathic remedies and acupuncture made a huge difference in my recovery process. Mental health services were also key for me and I would encourage folks to sign up if they can. The emotional experience of my condition was something I wasn't prepared for. Even after I started feeling better physically, I had anxiety. Seeing a therapist really helped me on my journey and in my growth.
Hopes for the Future of Heart Failure Care
I hope that access is expanded, not only in terms of testing and diagnosis but treatment. Especially within Black communities where individuals tend to be undiagnosed or underdiagnosed, despite being disproportionately impacted by heart disease. I want us to be in a place where we can focus on these communities and get them the best possible care. Putting more of an emphasis on patient experiences so patients can evaluate their care within the medical field and how they're being treated is also a hope of mine. By putting more accountability on the healthcare system, every patient can get the best care.
I would also love to see more emotional and mental health support connected to recovery. A way to foster this would be for hospitals to create more community-oriented spaces to connect patients who share similar health conditions. That sense of community was something I was missing while going through recovery and many communities don't heal in isolation.
The Importance of Having Support
I would be remiss if I didn't give a shoutout to my wife who has been my biggest support system through all of this. As much as I was dealing with at the time, she had to pick up the pieces where I couldn't. I want to underscore how important and invaluable she was in this process as well. She was the one who advocated for me in the emergency room to get all the testing so that my heart failure diagnosis could be caught. I believe she saved my life.
